|
Getting your Trinity Audio player ready...
|
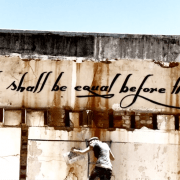
In May 2014 we reported on the start of the Competition Commission’s market inquiry into private healthcare. The healthcare market inquiry (HMI) was set up to probe the general state of competition in this sector to determine what can be done to make accessible, affordable, high quality and advanced private healthcare more widely available in South Africa.
Chaired by former Chief Justice Sandile Ngcobo, the inquiry would also determine how the market sets its prices, and ensure that the market allows for citizens’ constitutional right to access to healthcare.
Four years later, the commission has published its interim report, a weighty tome of 479 pages – but it is important to note that input from stakeholders is needed before a final version can be published.
As of 7 September 2018, the HMI had received 47 submissions and 17 requests for a submission extension, in response to its interim report.
Industry not well run
The panel’s overall assessment of the market was scathing: “… characterised by high and rising costs of healthcare and medical scheme cover, highly concentrated funders’ and facilities’ markets, disempowered and uninformed consumers, a general absence of value-based purchasing, ineffective constraints on rising volumes of care, practitioners that are subject to little regulation, and failures of accountability at many levels.”
The overall incomplete regulatory regime, the HMI panel noted, can largely be attributed to a failure in implementation on the part of regulators and inadequate stewardship by the Department of Health over the years.
The panel felt it important to mention that, although there is a perception that health care is of better quality in the private sector, this was difficult to assess objectively as there is no standard method of measuring or comparing the quality of outcomes or services, nor is there any measure of cost effectiveness in the private healthcare sector.
The lack of standardisation also extends to the benefits offered by schemes, so that for clients, picking one of the “22 open medical schemes and 185 benefit options that are neither standardised, nor comparable” is a daunting task.
Industry dominated and monopolised by a few
One of the HMI’s major findings is that there are a few main players in the private healthcare market in South Africa, who leave little room for anyone else. Economics professor Frederik Booysen of Wits University, in an analysis of the findings, writes that such an anti-competitive environment allows behaviour such as collusion and excessive pricing to thrive.
The two largest schemes together hold around 70% of the market. “One dominant open medical scheme, Discovery Health Medical Scheme (DHMS), comprises 55% of the open scheme market, and it continues to grow organically and through a series of amalgamations with smaller restricted schemes. The Government Employees Medical Scheme is the largest restricted scheme and is second only to DHMS as measured by number of beneficiaries.”
Not only is the medical cover sector dominated by these two schemes, but the private hospital sector also suffers from a lack of competition. “Three hospital groups, Netcare, Mediclinic and Life have a combined market share of 83% of the national South African private facilities market in terms of number of beds and 90% in terms of total number of admissions.” An admission is defined as any hospital consultation that incurred a facility fee payable to a hospital or hospital group.
As a result, there is little effective direct competition between the three big hospital groups. They can “continue in the knowledge that significant challenge is unlikely and this is probably the main reason the industry is not seeing innovation throughout the sector”.
This situation is exacerbated by the finding of “a significant positive correlation between risk of admission and having more doctors or hospital beds in that geography” and a similar significant positive correlation between the risk of admission to ICU and the number of ICU beds in a location.
The panel suggested that this observation, when combined with the fact that ICU admission rates are high by international standards, suggests that utilisation is at least partly driven by supply of doctors and facilities, rather than patient need.
This contributed to the high expenditure in private healthcare, which is increasing above inflation, making medical scheme premiums less affordable. “The bulk of this increase in claim expenditure can be attributed to expenditure on private hospitals and medical specialists,” the panel noted.
“The absolute level, and rate of increase of admissions in South Africa are, in combination, very worrying.”
Improving governance and boosting competition
The HMI’s preliminary recommendations were aimed at addressing harm to competition, Ngcobo said. “And these preliminary recommendations should form the basis of engagement on how best to address harm to competition that we have identified in our provisional findings. “
He cautioned that the recommendations must be viewed as a package, as a partial implementation will not address the failures identified by the HMI.
The HMI recommended, among others, that medical aid schemes be simplified with a “base benefit option that covers catastrophic expenditure as well as out-of-hospital preventative and primary care. The base benefit option should be standardised across schemes so that it is easy to compare and will be obligatory – all medical scheme members must purchase the base benefit option. “
The panel also made various recommendations to improve the governance of schemes and to ensure that schemes act in the interest of members in holding administrators to account. For instance, trustees’ and principal officers’ salaries should be explicitly linked to objective performance-based criteria. Furthermore, minimum education and training standards should be put in place for trustees and principal officers, and schemes should actively encourage their members to participle in annual general meetings.
For more findings, observations and recommendations, read the full interim report.